Acid reflux heartburns
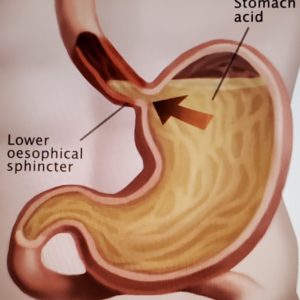
Photo caption:
The sphincter between the esophagus (foodpipe) and the stomach prevents digestive acid normally present in the stomach from “leaking” upwards to the esophagus. Among those with loose sphincter, this acid backs up (as shown by the arrow) to the esophagus and burns it (esophagitis), a situation commonly seen in patients with GERD.- From Spencer Sutton Science Source.
The COVID-19 pandemic has compounded the stress in people’s lives. One of the collateral side-effects is aggravation of existing psychologic and/or somatic conditions among individuals. This is exemplified by stress intensifying gastroesophageal reflux disease (GERD), which causes reflux heartburns.
What is reflux heartburns?
Reflux Heartburns is a milder stage of Reflux Esophagitis, which is an inflammatory condition where Hydrocholoric Acid, normally produced by the stomach to aid in the digestion of food, regurgitate (goes back up) to the lower end of the esophagus (food pipe) which is connected to the stomach. In most cases, the lower esophageal sphincter (“valve”) is incompetent (loose) and allows stomach acid and food to back up to the esophagus, a disease medically known as Gastroesophageal Reflux Disease (GERD).
Why is acid reflux bad?
The stomach mucosa (lining) normally produces the digestive acid and tolerates it much better than the esophagus, which has a different cell lining that is less resistant to the acid. Reflux of stomach acid into the lower end of the esophagus, therefore, causes esophagitis (irritation, inflammation and swelling), which, if allowed to continue untreated, could cause esophageal stricture (scarring) and narrowing, making the channel connecting the food pipe to the stomach too small for food to pass through, and even cancer.
Is this condition common?
Yes, very common. Most patients complain of burning discomfort in the pit of the stomach after meals or at night, while lying down, allowing stomach acid to flow back to the esophagus. Many times the burning disappears when the person gets up. The symptom could also be that of indigestion or “sour stomach.” People who take antacids, like Alka Seltzer, Maalox, Tums, etc. could have GERD.
Is Hiatal Hernia present in reflux esophagitis?
The food pipe, which is in the chest, goes down through a hole in the diaphram (the tent-like flat muscle that separates the abdomen from the chest) to connect with the stomach in the abdomen. This hole is called a hiatus. If this hole becomes too large, the stomach, which is normally in the abdomen, could move up to the chest through the hole. If this happens, it is called Hiatus Hernia. Hiatus Hernia is found in only 20-30% of those with reflux esophagitis. The majority do not have accompanying Hiatus Hernia.
Any other possible cause of esophagitis and stricture?
Caustic acids, or alkali (the chemical in Liquid Plumber, Sosa, etc.) when swallowed (as in suicides), cause massive burns, swelling, sometimes esophageal perforation (hole through the damaged foodpipe) and leads to severe esophagitis and esophageal stricture. The perforation could also result in Mediastinitis, a serious and overwhelming infection inside the chest, which has a high fatality or mortality rate. Chest surgery is usually carried out immediately the moment the diagnosis is made.
What are the possible complications of GERD?
Uncomplicated gastroesophageal reflux responds well to modern medical therapy, and may be tolerated for many years. However, some people on treatment may still develop complications, like esophagitis, esophageal ulcer, hemorrhage, esophageal stricture, and Barrett’s metaplasia (cell changes in the esophagus that could transform to cancer).
How is the diagnosis of GERD confirmed?
A careful history and thorough physical examination, coupled with X-Ray Barium Swallow (done with the patient on his back and the head lower than the feet to check for reflux of barium), esophageal monometry (pressure measurement), pH (acidity) monitoring, Bernstein acid test, and upper endoscopy (looking inside and down the foodpipe by passing a lighted “telescope” to see the condition of the lower foodpipe and stomach). Through this same scope, electro-cautery could be done to stop bleeding, and tiny biopsies could be performed, to see the tissue reaction and to check for cancer.
What is the first step treatment of GERD?
The initial management of patients with persisting symptoms of GERD consists of (1) Changing diet (avoiding alcohol, spices, caffeine, chocolate, alcohol, cola drinks), (2) quitting cigarette smoking, (3) avoiding tight, binding clothing, especially after a meal (4) refraining from lying down immediately after a meal, and elevating the head of the bed when lying down to keep gastric acid and contents in the stomach by gravity, and (5) taking regular Proton Pump Inhibitor (PPI) pills (like esomeprazole, etc.) under the close supervision of your physician.
If this treatment fails, then what?
If the initial therapy fails after 4 to 6 weeks, then endoscopy should be performed by your Gastroenterologist. More intensive treatment with PPI or H2 blocker to reduce acidity, use of bathanecol to raise the lower esophageal sphincter (LES) pressure to reduce reflux, or metoclopramide or cisapride to speed up gastric emptying into the small intestines. About 80 percent responds well to this therapy. However, this medication must be taken consistently under the care of your physician because recurrence is frequent with cessation of therapy.
When is surgery recommended?
When the strategic and intensive medical treatments enumerated above fail after several months to a year of trial, or when the PPI or H2Blocker pills are ineffective, or when the esophageal stricture does not stay open after dilatation, then surgery is recommended.
What is the objective of the operation?
The aim of the operation is to restore the anatomical and physiological condition in the lower end of the esophagus, as surgically possible, to minimize or prevent reflux of the gastric acid and content to the esophagus. If a bleeding esophageal ulcer and a stricture are present, then the surgeon will also address these accordingly.
How successful are these anti-reflux operations?
Very successful. Ten-year follow-up studies, some even longer, show that up to 90% of the patients are rendered asymptomatic (symptom-free), doing well, provided the changes in lifestyle recommended above were strictly followed.
COVID-19 Update
Worldwide, there are almost 38.3 million cases of COVID-19 and about 1.1 million deaths, 3352 new deaths in one day; Philippines, about 345,000, with 6,400 deaths; USA, almost 8.1 million, with about 221,000 deaths; India, 7,2 plus, almost 111,000 deaths; Brazil, 5.12 plus million cases, and 151,000 deaths. COVID-19 kills young and old alike, and using facemask properly and social distancing could significantly minimize the risk. Vigilance and a little healthy paranoia can spell the difference between getting infected or not. Be smart. Be safe.
The main objective of this column is to educate and inspire people live a healthier lifestyle to prevent illnesses and disabilities and achieve a happier and more productive life. Any diagnosis, recommendation or treatment in our article are general medical information and not intended to be applicable or appropriate for anyone. This column is not a substitute for your physician, who knows your condition well and who is your best ally when it comes to your health.



Leave a Reply